In 2018 Innovation Unit set out to enable people to recover and stay well in their communities. We were inspired by Living Well Lambeth, a person-centred, strengths-based, holistic approach to supporting people’s mental health. Our goal was to spread and scale the model across the UK, supported by the National Lottery Community Fund. You can read more about how our journey started in their report celebrating Three Decades of Making a Difference.
Seven years later, we’ve just finished our work scaling the Living Well (LW) approach across all ten localities in Greater Manchester.
What is Living Well?
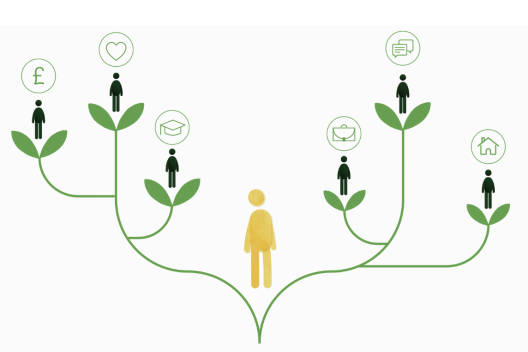
Living Well systems support people with complex needs who currently don’t get the help they need at the right time. Those who are ‘too complex’ for primary care and ‘not unwell enough’ for secondary care. Those who are on long waiting lists for limited, medicalised support that doesn’t take into account the social determinants impacting their mental health.
Instead, in a Living Well system, individuals are treated as whole people and active citizens. Multi-disciplinary teams combine skills and insights to deliver holistic, person-centred care, drawing on people’s strengths and lived experience. These systems are local, accessible, and community-rooted—each one shaped by its area. Support is easy to access and offered in everyday spaces. Staff are connected locally, and communities are actively involved in promoting mental wellbeing.
The recent publication of NHS England’s Neighbourhood Health Guidelines and upcoming NHS 10 year plan call for a shift from hospital to community and from sickness to prevention. It has never been clearer that there is a nationwide opportunity, and a mandate, to continue to change the way mental health support is delivered.
But changing systems while dealing with immense financial pressure and increasing demand is hard. Our work supports systems to tackle today’s urgent problems and grow sustainable solutions for the future.
Creating the environment for transformation
Building Leadership
Real change starts when leaders prioritise collaboration, learning, relationships and trust, moving away from systems which reward silos, gatekeeping and risk management. We built shared governance spaces which connected leaders across sectors and geographies and highlighted the experiences of people delivering and receiving support.
Leaders in these spaces were supported to tackle shared challenges, such as:
- Unpacking the data and digital barriers to sector partnerships
- Outlining an ideal approach for responding to risk and challenges in integrated teams
- Reflecting honestly on the role of lived experience across their offers.
In a recent survey, 100% of stakeholders (practitioners, system leaders, people with lived experience) agree or strongly agree that they have seen improved collaboration between sectors and organisations through this work.
“[Innovation Unit's] insightful approaches have allowed us to participate in a safe, well-held space within which we could challenge our assumptions and approaches in relation to lived experience involvement and co-production.”
Live Well leader
Real change starts when leaders prioritise collaboration, learning, relationships and trust, moving away from systems which reward silos, gatekeeping and risk management. We built shared governance spaces which connected leaders across sectors and geographies and highlighted the experiences of people delivering and receiving support.
Leaders in these spaces were supported to tackle shared challenges, such as:
- Unpacking the data and digital barriers to sector partnerships
- Outlining an ideal approach for responding to risk and challenges in integrated teams
- Reflecting honestly on the role of lived experience across their offers.
In a recent survey, 100% of stakeholders (practitioners, system leaders, people with lived experience) agree or strongly agree that they have seen improved collaboration between sectors and organisations through this work.
“[Innovation Unit's] insightful approaches have allowed us to participate in a safe, well-held space within which we could challenge our assumptions and approaches in relation to lived experience involvement and co-production.”
Live Well leader
Developing Practice
In order to develop integrated, multi-disciplinary teams providing preventative, person-centred and holistic care, practitioners must be empowered to change the way they work. In Greater Manchester, we held spaces for newly-formed teams to come together to shape a vision and values for mental health support that truly reflect their community’s strengths, needs, and identity. Teams were given the permission and processes to test out and learn from new ways of working to effectively meet the needs of their community. 100% of stakeholders (practitioners, system leaders, people with lived experience) agree or strongly agree that they have had more opportunities to try out new practice or ways of working as a result of Living Well.
We also convened a system wide Community of Practice (CoP) for statutory and VCSE neighbourhood teams. The space was pivotal in building shared practice, troubleshooting common challenges, and holding joint accountability.
“The CoPs have been a wonderful forum to share best practice and to feel connected.”
Practitioner involved in the programme
In order to develop integrated, multi-disciplinary teams providing preventative, person-centred and holistic care, practitioners must be empowered to change the way they work. In Greater Manchester, we held spaces for newly-formed teams to come together to shape a vision and values for mental health support that truly reflect their community’s strengths, needs, and identity. Teams were given the permission and processes to test out and learn from new ways of working to effectively meet the needs of their community. 100% of stakeholders (practitioners, system leaders, people with lived experience) agree or strongly agree that they have had more opportunities to try out new practice or ways of working as a result of Living Well.
We also convened a system wide Community of Practice (CoP) for statutory and VCSE neighbourhood teams. The space was pivotal in building shared practice, troubleshooting common challenges, and holding joint accountability.
“The CoPs have been a wonderful forum to share best practice and to feel connected.”
Practitioner involved in the programme
Connecting with Communities
Designing new models of community mental health support is not possible without meaningfully bringing local people together. In Greater Manchester we started with Collaboratives in each locality, open and inclusive spaces where anyone is welcome to play an active role in shaping the new offers.
The collaboratives brought residents, practitioners, commissioners, statutory providers, VCFSE organisations and people with lived experience together to co-design a model. We believe community mental health support is most successful when it both builds on the assets of a place and actively seeks to collaborate with underserved communities.
In a recent survey, 100% of stakeholders (practitioners, system leaders, people with lived experience) agree or strongly agree that they have seen more opportunities to put people receiving support at the centre of decision making through connecting with Living Well.
Designing new models of community mental health support is not possible without meaningfully bringing local people together. In Greater Manchester we started with Collaboratives in each locality, open and inclusive spaces where anyone is welcome to play an active role in shaping the new offers.
The collaboratives brought residents, practitioners, commissioners, statutory providers, VCFSE organisations and people with lived experience together to co-design a model. We believe community mental health support is most successful when it both builds on the assets of a place and actively seeks to collaborate with underserved communities.
In a recent survey, 100% of stakeholders (practitioners, system leaders, people with lived experience) agree or strongly agree that they have seen more opportunities to put people receiving support at the centre of decision making through connecting with Living Well.
A supported environment leads to significant impact
Creating an environment which supports meaningful transformation has led to significant impact for people, teams and communities:
Improved outcomes
In Salford, surveys measuring the experience of people accessing the Mental Health Neighbourhood team found that:
- 100% of people agree or strongly agree that the support they received has improved their wellbeing
- 91% agree or strongly agree that the care they received took into account their personal and social circumstances
- 55% experienced a reliable improvement in the Recovering and Quality of Life person level outcome measure.
Staff satisfaction in the Salford Mental Health Neighbourhood team is also much higher than local and national averages: 94% of staff would recommend their organisations as a place to work.
Collaborative services
An explicit focus on building an inclusive culture and shared practice in local areas enabled teams in Heywood, Middleton and Rochdale to partner with community organisations to strengthen their offer. Additional services they can now draw on include substance misuse and rough sleeper support. The team operates from GP practices, enabling a culture of reciprocal support that replaces referrals and hand-offs with truly collaborative care across primary and secondary care, and VCFSE partners.
"It’s good to talk to them [the Living Well professionals] and they’re really helpful. It’s good they link with my doctor and the nurse from Turning Point [substance misuse]. Everyone is working together to help me."HMR service user
Community connections
In Wigan, a borough with a long sporting history, the peer workforce led the development of the Game Changing Community Programme, working with Wigan Athletic Community Trust and BeWell (council leisure services). The programme is a trauma informed approach to introducing physical activity as wellbeing support into people’s lives. Each week includes a peer led session, a new physical activity to try, and a group gym session with a Personal Trainer. All sessions are hosted in community venues where participants can continue to access support.
"The gym programme has impacted me far beyond my physique. The main benefit I have noticed is not of my improving physical activity, but that of my mental wellbeing."Peer Led session attendee
Join our transformation community
Truly shifting community mental health systems is difficult work, but it is more important now than ever. Over the last 5 years there has been a 45% increase in the number of people in contact with secondary mental health services, 40% of people are waiting too long for care and workforce challenges remain fierce, with a vacancy rate across the mental health sector of 9.9%.
The time to change the way we offer mental health support is now.
We are building a community of change-makers who are as eager as we are to share learning, connect to other places already on their transformation journey, share best practice and work collaboratively to tackle barriers.
If you are transforming models of neighbourhood mental health in your area, we would love to connect.
Share this page